Bile Duct Cancer (Medicine Book 10)
Contents:
The extrahepatic bile duct is made up of the hilum region and the distal region. Cancer can form in either region: Risk factors for bile duct cancer include the following conditions: Primary sclerosing cholangitis a progressive disease in which the bile ducts become blocked by inflammation and scarring.
Cysts in the bile ducts cysts block the flow of bile and can cause swollen bile ducts, inflammation, and infection. Infection with a Chinese liver fluke parasite. Check with your doctor if you have any of the following: Jaundice yellowing of the skin or whites of the eyes. Pain in the abdomen. The following tests and procedures may be used: Physical exam and history: An exam of the body to check general signs of health, including checking for signs of disease, such as lumps or anything else that seems unusual.
A procedure in which a blood sample is checked to measure the amounts of bilirubin and alkaline phosphatase released into the blood by the liver. A higher than normal amount of these substances can be a sign of liver disease that may be caused by bile duct cancer. Medical procedures that test samples of tissue , blood, urine, or other substances in the body. These tests help to diagnose disease, plan and check treatment, or monitor the disease over time. A procedure in which a sample of blood, urine, or tissue is checked to measure the amounts of certain substances made by organs , tissues, or tumor cells in the body.
Certain substances are linked to specific types of cancer when found in increased levels in the body. These are called tumor markers. Higher than normal levels of carcinoembryonic antigen CEA and CA may mean there is bile duct cancer. A procedure in which high-energy sound waves ultrasound are bounced off internal tissues or organs, such as the abdomen, and make echoes. The echoes form a picture of body tissues called a sonogram.
The picture can be printed to be looked at later.
Bile Duct Cancer
CT scan CAT scan: A procedure that makes a series of detailed pictures of areas inside the body, such as the abdomen, taken from different angles. The pictures are made by a computer linked to an x-ray machine. A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography. MRI magnetic resonance imaging: A procedure that uses a magnet, radio waves , and a computer to make a series of detailed pictures of areas inside the body.
This procedure is also called nuclear magnetic resonance imaging NMRI. MRCP magnetic resonance cholangiopancreatography: A procedure that uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the body such as the liver, bile ducts, gallbladder, pancreas, and pancreatic duct. Types of biopsy procedures include the following: A surgical procedure to look at the organs inside the abdomen, such as the bile ducts and liver, to check for signs of cancer.
Small incisions cuts are made in the wall of the abdomen and a laparoscope a thin, lighted tube is inserted into one of the incisions. Other instruments may be inserted through the same or other incisions to perform procedures such as taking tissue samples to be checked for signs of cancer.
Percutaneous transhepatic cholangiography PTC: A procedure used to x-ray the liver and bile ducts.
- Cholangiocarcinoma (bile duct cancer) - Symptoms and causes - Mayo Clinic.
- .
- La Source Op.23 - Harp;
- .
A thin needle is inserted through the skin below the ribs and into the liver. Dye is injected into the liver or bile ducts and an x-ray is taken. A sample of tissue is removed and checked for signs of cancer. If the bile duct is blocked, a thin, flexible tube called a stent may be left in the liver to drain bile into the small intestine or a collection bag outside the body. This procedure may be used when a patient cannot have surgery.
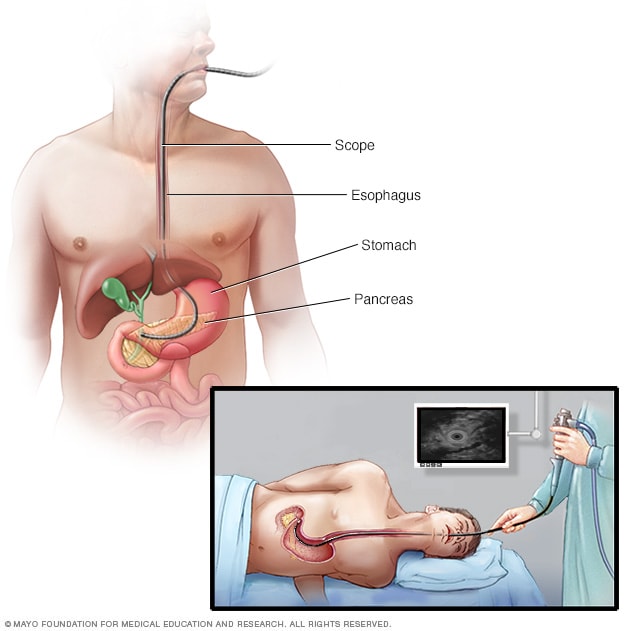
Endoscopic retrograde cholangiopancreatography ERCP: A procedure used to x-ray the ducts tubes that carry bile from the liver to the gallbladder and from the gallbladder to the small intestine. Sometimes bile duct cancer causes these ducts to narrow and block or slow the flow of bile, causing jaundice. An endoscope is passed through the mouth and stomach and into the small intestine.
Dye is injected through the endoscope thin, tube-like instrument with a light and a lens for viewing into the bile ducts and an x-ray is taken. If the bile duct is blocked, a thin tube may be inserted into the duct to unblock it. This tube or stent may be left in place to keep the duct open. A procedure in which an endoscope is inserted into the body, usually through the mouth or rectum.
An endoscope is a thin, tube-like instrument with a light and a lens for viewing. A probe at the end of the endoscope is used to bounce high-energy sound waves ultrasound off internal tissues or organs and make echoes. This procedure is also called endosonography.
The prognosis chance of recovery and treatment options depend on the following: Whether the cancer is in the upper or lower part of the bile duct system. The stage of the cancer whether it affects only the bile ducts or has spread to the liver, lymph nodes , or other places in the body.

Whether the cancer has spread to nearby nerves or veins. Whether the cancer has just been diagnosed or has recurred come back. Cancer may spread from where it began to other parts of the body. Stages are used to describe the different types of bile duct cancer. The results of diagnostic and staging tests are used to find out if cancer cells have spread. There are three ways that cancer spreads in the body. Cancer can spread through tissue , the lymph system , and the blood: The cancer spreads from where it began by growing into nearby areas.
The cancer spreads from where it began by getting into the lymph system. The cancer travels through the lymph vessels to other parts of the body.
The cancer spreads from where it began by getting into the blood. The cancer travels through the blood vessels to other parts of the body. The cancer gets into the lymph system, travels through the lymph vessels, and forms a tumor metastatic tumor in another part of the body. The cancer gets into the blood, travels through the blood vessels, and forms a tumor metastatic tumor in another part of the body. Intrahepatic bile duct cancer Stage 0: In stage 0 intrahepatic bile duct cancer, abnormal cells are found in the innermost layer of tissue lining the intrahepatic bile duct.
These abnormal cells may become cancer and spread into nearby normal tissue.
Buy Bile Duct Cancer (Medicine Book 10): Read Books Reviews - www.farmersmarketmusic.com Bile Duct Cancer: Symptoms, Treatment and Prognosis: Medicine & Health Science Books @ www.farmersmarketmusic.com ISBN X; ISBN ; Product Dimensions: x x inches; Shipping Weight.
Stage 0 is also called carcinoma in situ. In stage II intrahepatic bile duct cancer, either of the following is found: In stage IV intrahepatic bile duct cancer, cancer has spread to other parts of the body, such as the bone, lungs , distant lymph nodes , or tissue lining the wall of the abdomen and most organs in the abdomen.
Perihilar bile duct cancer Stage 0: In stage 0 perihilar bile duct cancer , abnormal cells are found in the innermost layer of tissue lining the perihilar bile duct. Stage 0 is also called carcinoma in situ or high-grade dysplasia. In stage I perihilar bile duct cancer , cancer has formed in the innermost layer of tissue lining the perihilar bile duct and has spread into the muscle layer or fibrous tissue layer of the perihilar bile duct wall.
In stage II perihilar bile duct cancer , cancer has spread through the wall of the perihilar bile duct to nearby fatty tissue or to liver tissue. Distal extrahepatic bile duct cancer Stage 0: In stage 0 distal extrahepatic bile duct cancer , abnormal cells are found in the innermost layer of tissue lining the distal extrahepatic bile duct. In stage I distal extrahepatic bile duct cancer , cancer has formed and spread fewer than 5 millimeters into the wall of the distal extrahepatic bile duct.
Cancer has spread 5 millimeters or more into the wall of the distal extrahepatic bile duct. Cancer may have spread to 1 to 3 nearby lymph nodes. In stage IV distal extrahepatic bile duct cancer , cancer has spread to other parts of the body, such as the liver , lungs , or tissue lining the wall of the abdomen and most organs in the abdomen. The following groups are used to plan treatment: Resectable localized bile duct cancer The cancer is in an area, such as the lower part of the common bile duct or perihilar area, where it can be removed completely by surgery.
Unresectable, metastatic, or recurrent bile duct cancer Unresectable cancer cannot be removed completely by surgery. Patients can enter clinical trials before, during, or after starting their cancer treatment. There are different types of treatment for patients with bile duct cancer. Three types of standard treatment are used: Surgery The following types of surgery are used to treat bile duct cancer: Removal of the bile duct: A surgical procedure to remove part of the bile duct if the tumor is small and in the bile duct only.
Lymph nodes are removed and tissue from the lymph nodes is viewed under a microscope to see if there is cancer. A surgical procedure in which the part of the liver where cancer is found is removed. The part removed may be a wedge of tissue, an entire lobe , or a larger part of the liver, along with some normal tissue around it. A surgical procedure in which the head of the pancreas , the gallbladder , part of the stomach , part of the small intestine , and the bile duct are removed.
Enough of the pancreas is left to make digestive juices and insulin. If cancer is blocking the bile duct and bile is building up in the gallbladder, a biliary bypass may be done. During this operation, the doctor will cut the gallbladder or bile duct in the area before the blockage and sew it to the part of the bile duct that is past the blockage or to the small intestine to create a new pathway around the blocked area.
If the tumor is blocking the bile duct, surgery may be done to put in a stent a thin tube to drain bile that has built up in the area. The doctor may place the stent through a catheter that drains the bile into a bag on the outside of the body or the stent may go around the blocked area and drain the bile into the small intestine.
Percutaneous transhepatic biliary drainage: Radiation therapy Radiation therapy is a cancer treatment that uses high-energy x-rays or other types of radiation to kill cancer cells or keep them from growing.
- .
- .
- Turn Me Loose: The Unghosting of Medgar Evers!
- Cholangiocarcinoma (bile duct cancer) - Diagnosis and treatment - Mayo Clinic?
- Green Abyss!
- .
- .
Select Slot Select time. Home Type of cancers Bile Duct Cancer. Overview Symptoms Causes Diagnosis Treatment. Overview Bile duct cancer starts in the bile duct. Cancers can develop in any part of the bile duct and, based on their location, are classified into three types: They can sometimes be confused with cancers that start in the liver cells, which are called hepatocellular carcinomas, and are often treated the same way. Only about 1 in 10 bile duct cancers are intrahepatic.
They are also called Klatskin tumours. These are the most common type of bile duct cancers, making up 6 or 7 of every 10 bile duct cancers. These cancers are grouped with distal bile duct cancers as extrahepatic bile duct cancers. Distal bile duct cancers make up 2 to 3 of every 10 bile duct cancers. Symptoms Signs and symptoms may not be present until the later stages of bile duct cancer, but in some cases they may lead to an early diagnosis. The following are some symptoms associated with bile duct cancer: Conditions that are associated with this kind of inflammation include: Diagnosis Bile duct cancer can be a challenging condition to diagnose.
Some of the tests are described below: These types of proteins are known as tumour markers. However, tumour markers can also be caused by other conditions. A positive blood test does not necessarily mean that the patient is suffering from bile duct cancer, and vice versa. The x-ray scanner is used to guide an endoscope down the throat and into your bile duct.
The endoscope can detect blockages in the bile duct, which could actually indicate bile duct cancer. This involves passing a specialised endoscope into the bile duct so that abnormalities if any, can be spotted. It also enables a biopsy to be taken at this stage.
Turn recording back on. In stage 0 perihilar bile duct cancer , abnormal cells are found in the innermost layer of tissue lining the perihilar bile duct. The histologic types of perihilar bile duct cancer include the following: In jaundiced patients, the role of percutaneous transhepatic catheter drainage or endoscopic placement of a stent for relief of biliary obstruction is controversial, but may be considered before surgery, particularly if jaundice is severe or an element of azotemia is present. Turn recording back on. When chemotherapy is taken by mouth or injected into a vein or muscle, the drugs enter the bloodstream and can reach cancer cells throughout the body systemic chemotherapy. Mayo Foundation for Medical Education and Research;
During a biopsy, a small sample of tissue is taken from the body and checked under a microscope for the presence of cancerous cells. As well as taking bile and tissue samples from the bile duct, samples may be taken from nearby lymph nodes. This is to check whether the cancer has spread from your bile duct into the lymphatic system.
Treatment Most cases of bile duct cancer cannot be cured. Depending on the extent of the cancer, it may be necessary to remove: This will help resolve symptoms such as: Two types of radiotherapy are used to treat bile duct cancer: Side effects of radiotherapy include: Side effects of chemotherapy can include: Cancer of the bile duct also called cholangiocarcinoma is extremely rare.
The true incidence of bile duct cancer is unknown, however, because establishing an accurate diagnosis is difficult. Traditionally, bile duct tumors located within the liver have been classified with hepatocellular carcinoma as primary liver tumors. Many bile duct cancers are multifocal. In most patients, the tumor cannot be completely removed by surgery and is incurable. Palliative measures such as resection, radiation therapy e. The biliary system consists of a network of ducts that carry bile from the liver to the small bowel and is classified by its anatomic location Figure 1.
Bile is produced by the liver and is important for fat digestion.
PDQ Cancer Information Summaries [Internet].
The bile ducts located within the liver are called intrahepatic bile ducts. Tumors of the intrahepatic bile ducts originate in small intrahepatic ductules or large intrahepatic ducts that are proximal to the bifurcation of the right and left hepatic ducts. These tumors are also known as intrahepatic cholangiocarcinomas. The bile ducts located outside of the liver are called extrahepatic bile ducts. They include part of the right and left hepatic ducts that are outside the liver, the common hepatic duct, and the common bile duct. The extrahepatic bile ducts can be further divided into the perihilar hilum region and distal region.
Bile duct cancer may occur more frequently in patients with a history of primary sclerosing cholangitis, chronic ulcerative colitis, choledochal cysts, or infections with the liver fluke Clonorchis sinensis. Distal extrahepatic and perihilar bile duct cancers frequently cause biliary tract obstruction, leading to the following symptoms:. Intrahepatic bile duct cancer may be relatively indolent and difficult to clinically differentiate from metastatic adenocarcinoma deposits in the liver.
Clinical evaluation is dependent on laboratory and radiographic imaging tests that include the following:. These tests demonstrate the extent of the primary tumor and help determine the presence or absence of distant metastases. If a patient is medically fit for surgery and the tumor is amenable to surgical resection, surgical exploration is performed. Pathologic examination of the resected specimen is done to establish definitive pathologic staging. Because of its nearness to major blood vessels and diffuse extension within the liver, a bile duct tumor can be difficult to resect.
Complete resection with negative surgical margins offers the only chance of cure for bile duct cancer. For localized, resectable extrahepatic and intrahepatic tumors, the presence of involved lymph nodes and perineural invasion are significant adverse prognostic factors. Additionally, the following have been associated with worse outcomes among patients with intrahepatic cholangiocarcinomas: Other PDQ summaries containing information related to bile duct cancer include the following:.
The most common histopathologic types of intrahepatic bile duct tumor include the following: Adenocarcinomas are the most common type of perihilar bile duct tumor. The histologic types of perihilar bile duct cancer include the following: Adenocarcinomas are the most common type of distal extrahepatic bile duct tumors. The histologic types of distal extrahepatic bile duct cancer include the following: Bile duct cancer is classified as resectable localized or unresectable, with obvious prognostic importance.
The TNM tumor, node, metastasis staging system is used for staging bile duct cancer, commonly after surgery and pathologic examination of the resected specimen. Evaluation of the extent of disease at laparotomy is an important component of staging. Tables 1 , 2 , 3 , 4 , and 5 pertain to the intrahepatic bile duct cancer stages. View in own window. Tables 6 , 7 , 8 , 9 , and 10 pertain to the perihilar bile duct cancer stages. Tables 11 , 12 , 13 , 14 , 15 pertain to the distal extrahepatic bile duct cancer stages.
The treatment of bile duct cancer depends primarily on whether the cancer can be completely removed by surgery. Localized intrahepatic and extrahepatic bile duct cancer may be removed completely by the surgeon. These tumors represent a very small number of cases that are usually in the distal common bile duct. Among patients treated with surgical resection, long-term prognosis varies depending on primary tumor extent, margin status, lymph node involvement, and additional pathologic features. Extended resections of hepatic duct bifurcation tumors Klatskin tumors, also known as hilar tumors to include adjacent liver, either by lobectomy or removal of portions of segments 4 and 5 of the liver, may be performed.
If major hepatic resection is necessary to achieve a complete resection, postoperative hepatic reserve should be evaluated. Most cases of intrahepatic, extrahepatic, and perihilar bile duct cancer are unresectable and cannot be completely removed by the surgeon. Often the cancer invades directly into the portal vein, the adjacent liver, along the common bile duct, and to adjacent lymph nodes. Portal hypertension may result from invasion of the portal vein.
Spread to distant parts of the body is uncommon, but intra-abdominal metastases, particularly peritoneal metastases, do occur. Transperitoneal and hematogenous hepatic metastases also occur with bile duct cancer of all sites. Moreover, most patients who undergo resection will develop recurrent disease within the hepatobiliary system or, less frequently, at distant sites.
For patients with unresectable bile duct cancer, management is directed at palliation. Treatment options for bile duct cancer are described in Table Standard treatment options for resectable intrahepatic bile duct cancer include the following:. For intrahepatic bile duct cancers, hepatic resection to achieve negative margins is the curative procedure. If a major liver resection is necessary to achieve negative surgical margins, preoperative portal vein embolization may be considered to increase the volume of the remnant liver.
Partial liver resection or partial hepatectomy to achieve negative margins is the mainstay of cure for patients with intrahepatic cholangiocarcinoma. The role of routine portal lymphadenectomy has not been well established because of the risk of common bile duct devascularization. Use our advanced clinical trial search to find NCI-supported cancer clinical trials that are now enrolling patients. The search can be narrowed by location of the trial, type of treatment, name of the drug, and other criteria. General information about clinical trials is also available.
Standard treatment options for unresectable, recurrent, or metastatic intrahepatic bile duct cancer include the following:. Relief of biliary obstruction is warranted when symptoms such as pruritus and hepatic dysfunction outweigh other symptoms of the cancer. When possible, such palliation can be achieved with the placement of bile duct stents by operative, endoscopic, or percutaneous techniques.
Palliative radiation therapy may be beneficial, and patients may be candidates for inclusion in clinical trials that explore ways to improve the effects of radiation therapy with various radiation sensitizers, such as hyperthermia, radiosensitizer drugs, or cytotoxic chemotherapeutic agents. If a percutaneous catheter has been placed, it can be used as a conduit for placement of brachytherapy sources. Systemic chemotherapy is appropriate for selected patients with adequate performance status and intact organ function. The following agents have been reported to produce transient partial remissions in a minority of patients:.
A phase III study NCT randomly assigned patients with unresectable, recurrent, or metastatic biliary tract carcinoma to receive cisplatin followed by gemcitabine or to receive gemcitabine alone for up to 6 months and observed the following: Patients with unresectable, recurrent, or metastatic bile duct cancer should be considered for inclusion in clinical trials whenever possible. Information about ongoing clinical trials is available from the NCI website. Standard treatment options for resectable perihilar bile duct cancer include the following:.
For perihilar cholangiocarcinomas Klatskin tumors , bile duct resection alone leads to high local recurrence rates resulting from the early confluence of the hepatic ducts and the caudate lobe. The addition of partial hepatectomy that includes the caudate lobe has improved long-term outcomes but may be associated with increased postoperative complications. The primary site of relapse after surgical resection is local; however, distant recurrence has been frequently reported. However, radiation therapy external-beam radiation therapy [EBRT] with or without brachytherapy has been reported to improve local control.
The optimal surgical procedure for carcinoma of the perihilar bile duct varies according to the location of the tumor along the biliary tree, the extent of hepatic parenchymal involvement, and the proximity of the tumor to major blood vessels in this region. The state of the regional lymph nodes is assessed at the time of surgery because of their prognostic significance. In jaundiced patients, the role of percutaneous transhepatic catheter drainage or endoscopic placement of a stent for relief of biliary obstruction is controversial because of inconsistent findings of significant clinical benefit and concerns of increased risk of postoperative complications.