Pathways to Pain Relief
Contents:
The pathway recommends that commissioners should ensure structured education with appropriate resources in place.
Information that patients require is diverse. It is unclear how much patients benefit from structured education, but by extrapolating from diabetes care, cancer pain, treatment for alcohol dependency, and learning from the Expert Patient Programme experience, it is clear that a proportion will benefit. However, those at a higher risk of more severe impact of pain on their lives are likely to require a more significant investment—individualized care plans are often advocated in this circumstance.
Pathways to Pain Relief
There are a myriad of definitions pertaining to acute and chronic pain. These cause confusion in terms of both clinical management and service delivery. Pain of a short duration has less impact on the individual, and thus a single practitioner could be expected to reasonably manage most episodes. Severe enduring pain may require a whole team to support the patient. Identification of psychosocial factors that may increase pain and associated disability are also critical; these will prolong pain problems. The guidance will need to be updated to reflect the emerging consensus on terminology.
Coding practices are also likely to require a review to ensure that the terminology is consistent. A purely biomedical perspective is unlikely to get to the bottom of why pain persists in many people. The pathway highlights that an assessment may be difficult because pain can be complex with entwined physical and psychosocial factors.
For health professionals supporting chronic pain self management
At a pathological level, systemic diseases may be masked by changes in pain, development of new problems, and psychological issues. Getting the balance right is essential for a successful outcome. Research has highlighted that patients may not present with pain but with its consequences such as: The pathway group recommends simple tests and nothing more in the initial assessment and management of pain. For example, X-rays to exclude trauma and erythrocyte sedimentation rate for suspected inflammatory disease are regarded as sufficient initial investigations.
This list is not exhaustive, and the important point is to move away from the continuous cycle of investigations and encourage non-specialists to utilize a bio-psychosocial assessment for management. The pathway contains a list of recommendations on how to identify those at risk of chronic disability and suggests psychosocial interventions that may reduce disability. While there has been extensive research into this for chronic back pain, the situation is less clear for other types of pain.
High-risk patients are offered a cognitive behavioural therapy CBT -based intervention with physical therapy, whereas the low-risk respondents are initially just given advice; it is a good example of how a risk assessment coupled with matched treatments may provide timely and cost-effective care. Other interventions include ensuring a strong therapeutic alliance and shared decision-making. While this is the bedrock of a consultation in primary care, the relationship between the specific format of a patient-centred consultation and the outcome is unclear and further work is needed on this.
Screenshots
Equally, there can be too much focus on psychosocial factors if they are readily identified, and the medical factors then get overlooked. A collaborative care model, which includes a two-session clinician education programme, patient assessment, education and activation, symptom monitoring, feedback and recommendations to clinicians, and facilitation of specialty care, has been shown to have promise in patients with musculoskeletal chronic pain.
Research is urgently needed into the nature and style of a pain-related consultation that can best deliver successful outcomes earlier in the patient journey. Active patient involvement in care requires a strong relationship and an information exchange in line with patient values and preferences. This can be formalized into a process known as shared decision making SDM. An example of such interventions is the patient decision aid, which breaks down decision-making into sequential steps while at the same time tries to elicit patient values and preferences.
These complex interventions have recently been developed to suit a range of decision-making styles in areas relevant to Pain Medicine. SDM has been found to improve patient satisfaction. However, SDM's impact on clinical outcomes and unwarranted variation is less clear.
Does your pain change with your mood or environment? This pathway focuses on the start of the journey of a patient with pain, where a full diagnostic work-up is not yet complete. Map of Medicine Care Map, which can be found at www. Thanks for telling us about the problem. You are commenting using your Twitter account. Initial assessment and management of pain: Much of the research is now looking at the changes in the brain, spinal cord and peripheral nervous sytems that are associated with chronic pain.
A useful mnemonic contained within the pathway is the concept of the four A's for effective treatment monitoring: Aberrant drug taking addiction-related outcomes. Trials of analgesia accompanied by close monitoring are recommended, with the imperative to stop if there is no or little response. The four A's approach provides a useful method to achieve this with timing matched to need. The awareness of the likelihood of analgesia failure needs to be raised with the general population and, rather than just discarding analgesia, persistence needs to be encouraged.
Imaginative solutions will be needed to deliver this recommendation, perhaps making better use of pharmacists, although a recent small randomized controlled trial had mixed results. The pathway group recommends additional interventions for those identified at high risk of chronicity. Enquiry into patient beliefs and expectations are fundamental to this. This provides a neccesary survival function since it allows the pain experience to be altered according to the situation rather than having pain always dominate [11].
Firstly, it helps physiotherapists explain why the amount of pain a patient is experiencing does not neccesarily relate to the amount of tissue damage they have sustained [10]. Neuroscience education has been shown to be effective in several studies [12] [13] [14] [15] [16] [17].
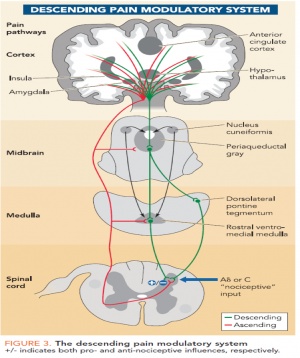
This knowledge can aid the physiotherapist with careful selection and use of techniques with a "top down" philosphy, freeing them from selecting interventions based merely on proposed local tissue reponses such as inhibiting reflex muscle contraction, reducing intra-articular pressure and reducing the level of joint afferent activity [21]. References will automatically be added here, see adding references tutorial.
The content on or accessible through Physiopedia is for informational purposes only. Physiopedia is not a substitute for professional advice or expert medical services from a qualified healthcare provider. Toggle navigation p Physiopedia. Contents Editors Categories Share Cite.
Opioids for pain relief in palliative care overview
We use cookies to give you the best possible experience. By using our website you agree to our use of cookies.
- Historical Dictionary of the Civil War (Historical Dictionaries of War, Revolution, and Civil Unrest).
- Brindle - Scryer Extraordinare!
- Monster: 1.
Dispatched from the UK in 3 business days When will my order arrive? Home Contact Us Help Free delivery worldwide. Pathways to Pain Relief. Description Based upon the pioneering work of John E. Sarno, MD, Pathways to Pain Relief offers the stories of seventeen patients who recovered from back pain, sciatica, and other pain disorders which were emotional in origin These stories are shared to help people searching for relief from pain and those who support them